News
How UNFPA helps mothers around the world embrace their right to good health and safe pregnancy
- 05 April 2024
News
UNITED NATIONS, New York – Everyone has the right to health; and for women and girls, one aspect of this fundamental promise is the right to safe motherhood.
Yet every two minutes, a woman or girl still dies due to pregnancy or childbirth, with the vast majority of these tragedies preventable. “It is unacceptable that so many women continue to die needlessly,” said Dr Natalia Kanem, Executive Director of UNFPA, the United Nations sexual and reproductive health agency, in 2023.
The world has achieved significant reductions in global maternal mortality, which dropped by more than a third between 2000 and 2020. But progress has slipped in recent years – a new development with age-old drivers – namely, systemic barriers to health.
Pregnancy and childbirth are less safe where women cannot get the care they need from providers like midwives, or where they must confront discrimination and bias when trying to access services. UNFPA research, for example, reveals that pregnancy and childbirth are more dangerous for Afrodescendent women and girls in the Americas due to mistreatment and neglect by health-care systems – itself a legacy of systemic racism.
But progress is possible, especially where countries invite marginalized communities to the table and tailor prevention programming to their needs. On this World Health Day, learn how UNFPA is working to safeguard the lives of mothers around the world so that women and girls are empowered to embrace health and experience pregnancy and childbirth as a time to thrive, not just survive.
Saving time and lives in Bangladesh
Over the last two decades, Bangladesh has achieved stunning reductions in maternal mortality, with the rate dropping by more than 70 per cent between 2000 and 2020.
Yet thousands of women are still dying preventable deaths each year, many due to delays in accessing care. Research indicates one in five maternal deaths in Bangladesh happen while a woman is in transit, pointing to potential issues with the country’s referral systems. When patients urgently need higher-level care, a lack of emergency transport or difficulties coordinating transfers can be deadly.
These issues could have presented problems for mother-of-three Majeda Begum, who faced complications while giving birth to her fourth child at a Dhaka maternity centre last year. But with support from a new app launched in 2020, Ma-Jaan, her seamless referral to a nearby hospital ended with a safe delivery via Caesarean section. As of 2023, the app had supported the transfer of more than 2,700 complex cases to referral institutions.
Ma-Jaan was developed as part of a UNFPA-supported initiative to provide low-income women with timely access to emergency obstetric services. It works by matching patients with nearby hospitals where they can receive care and helps with the logistics of referrals; for instance, Ms. Begum’s transport by autorickshaw to the hospital was arranged through the app.
As part of the project, health workers also make house calls. Ms. Begum told UNFPA that a health worker associated with the programme visited her home to conduct check-ups, perform tests and prescribe medication prior to her delivery. “This service is very useful for poor people like us,” she told UNFPA.
Fulfilling the right to health in Brazil
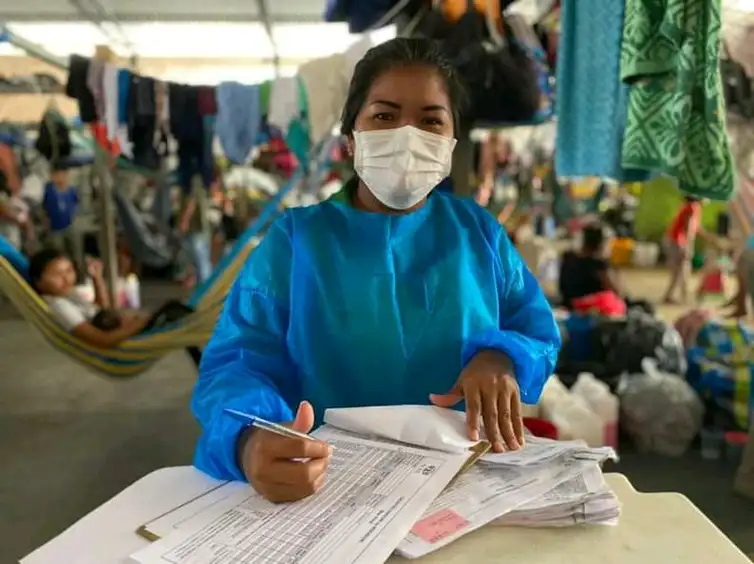
“[Preventing pregnancy] is not about restricting our tradition and culture; it’s about taking care of our children,” said Venezuelan doctor Fiorella Lisenni Ramos Blanco.
Dr. Blanco, a member of the Warao indigenous ethnic group, left Venezuela in 2019 for Brazil amid her home country’s escalating economic and political crisis. The turmoil has been particularly hazardous for women and girls; between 2015 and 2016, maternal deaths in the country spiked by 65 per cent.
But displacement can also be dangerous for women’s health, as it disrupts access to essential medicine and services. In Brazil, research indicates that family planning has remained out of reach for many Venezuelan migrants, an issue that can escalate risks of preventable maternal mortality.
Dr. Blanco noted the significance of access to family planning in Brazil while recognizing that indigenous women are sometimes culturally expected to have multiple children. “I think we are not in a place – economically or in terms of stability, especially in terms of housing – to be able to [provide] a better life for our children,” she said.
Under Brazil’s unified public health-care system, every person – including all Venezuelan migrants and refugees – can access a range of health services free of charge, including those related to sexual and reproductive health and rights. Today, the government is working to expand access to related services across states like Amazonas, in the country’s northwest.
Shádia Fraxe, municipal health secretary for the state’s capital, Manaus, told UNFPA that provision of intrauterine devices, for instance, has widened beyond the area’s maternity hospital to more than a dozen other health centres.
“We promote family planning,” Ms. Fraxe said. “Women were able to say ‘No, doctor, I don't want to have children anymore’, or ‘I want to plan my pregnancy’.”
“Information is the secret to everything,” she added.

Training midwives in Niger
Home to more than 35,000 people, the rural and remote canton of Déoulé in Niger is not an easy place to access health care. Nor is it a place where safety during pregnancy and childbirth is guaranteed, despite decades of progress that have cut Niger’s maternal mortality rate in half.
One problem is a lack of providers, according to Déoulé’s chief, Elhadji Mahaman Kadri Magori. Many health workers come to the area on contract, and few remain long term. “We needed health workers who would stay with us to take care of the population,” Mr. Magori told UNFPA.
Seeking a way to home-grow health workers, in 2020 the chief decided to sponsor the health studies of more than a dozen young women from his canton. The initiative served interrelated aims: To keep Déoulé’s girls in school for longer, and to expand and improve the canton’s health services.
Several of the sponsored students have already graduated from basic health training and moved on to specialize in midwifery. According to UNFPA, addressing the global shortage of midwives could prevent two thirds of maternal deaths.
''It is a source of pride for us to see our daughters working in the local health centres. It motivates us to go,” said Zeinabou, a housewife in Déoulé. “It's really wonderful.”